I’ve been in that spot, dealing with an infection, on antibiotics, and still craving a cigarette. If you’re anything like I was, you’ve probably wondered: Is it that bad to smoke while on antibiotics? The urge is real, but so are the risks.
This isn’t just a hypothetical concern. Smoking impacts your immune system, your lungs, and even how medications work in your body. I’ve talked to doctors, dug through research, and experienced the frustration of slow recovery firsthand. And trust me, what you do while on antibiotics can make a big difference.
In this article, I’ll break down what happens when you mix smoking and antibiotics. We’ll cover how smoking affects the healing process, which medications it interferes with, and what health experts recommend. By the end, you’ll have the facts you need to decide whether lighting up is worth the risk during treatment.
Understanding Antibiotics and Their Side Effects
Antibiotics fight infections but can cause side effects like nausea, diarrhea, or allergies. Knowing how they work helps manage risks.
What Are Antibiotics and How They Work

Antibiotics are powerful medicines that fight bacterial infections in your body. Think of them as targeted weapons against harmful bacteria. When I take an antibiotic, it works in one of two ways. It either kills bacteria directly or stops them from growing and multiplying.
Pretty straightforward, right? Common types you might recognize include:
- Amoxicillin for ear infections
- Doxycycline for skin conditions
- Azithromycin for respiratory issues
- Penicillin for strep throat
Here’s something important: antibiotics only work against bacteria. They’re completely useless against viruses like the common cold or flu. That’s why your doctor won’t prescribe them for every illness.
Common Antibiotic Side Effects
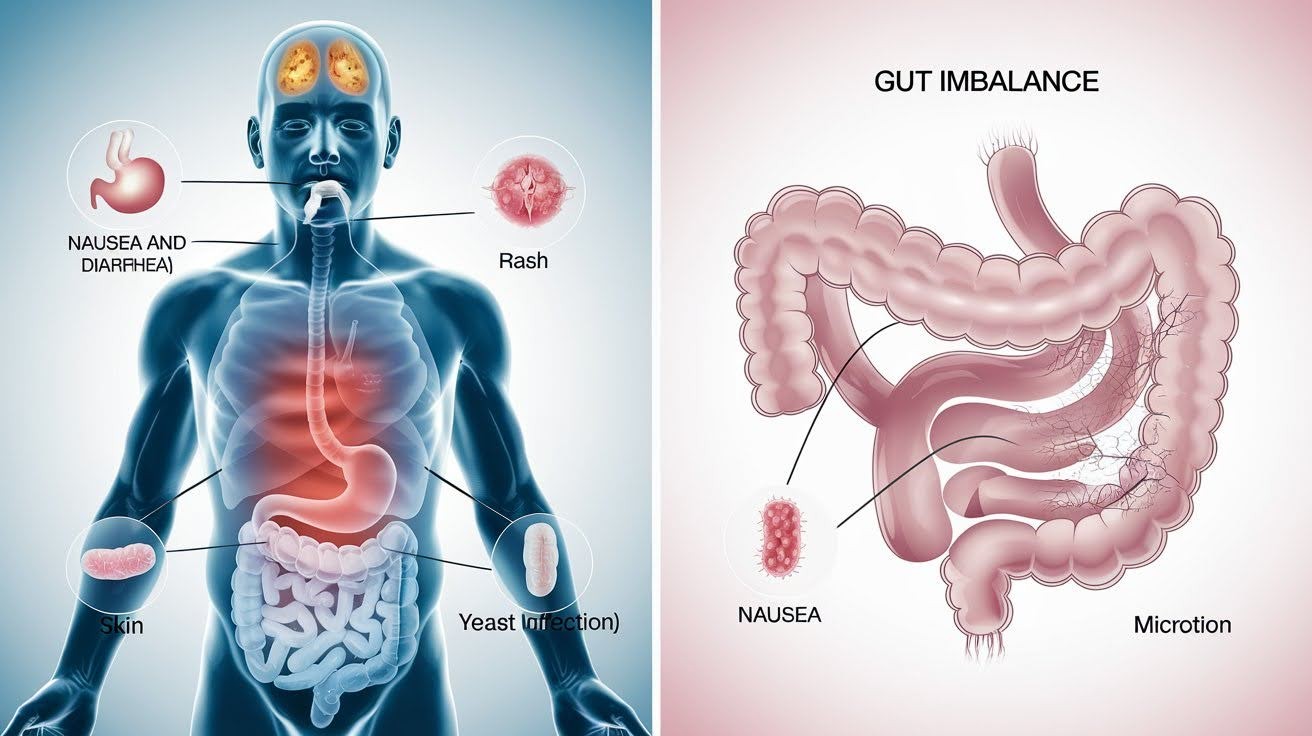
Even helpful medicines come with risks. I’ve experienced some of these myself. Short-term side effects happen quickly:
- Stomach upset and diarrhea
- Nausea that makes eating difficult
- Skin rashes or itching
- Yeast infections in women
But wait, there’s more to consider. Long-term concerns develop over time. Your gut contains millions of good bacteria that help digestion.
Antibiotics can wipe out these helpful microbes along with the bad ones. This creates an imbalance. Your immune system may weaken. Recovery takes longer than expected. That’s exactly why following your doctor’s instructions matters so much for getting better.
The Safety of Smoking Cannabis While Taking Antibiotics
Mixing cannabis with antibiotics raises safety concerns. Interactions may affect healing, side effects, or drug effectiveness. Caution is recommended.
Current Research Findings

When I started researching cannabis and antibiotics, I found something surprising. There’s very little direct research on this specific combination. Most major medical databases don’t list cannabis as having serious interactions with common antibiotics.
That’s different from other substances like alcohol or certain supplements. Here’s what the science shows so far:
- No documented dangerous reactions between cannabis and standard antibiotics
- Cannabis doesn’t appear on most drug interaction warning lists
- Limited studies suggest general safety for typical antibiotic courses
But here’s the catch. “Limited research” doesn’t mean “completely safe.” The absence of reported problems isn’t the same as proven safety.
Most doctors simply don’t have enough data to give you a definitive answer. The research just isn’t there yet. That’s why many healthcare providers take a cautious approach when you ask about mixing the two.
Specific High-Risk Antibiotics

Not all antibiotics are created equal when it comes to cannabis interactions. Some require more caution than others. Macrolide antibiotics top the concern list. These include erythromycin, clarithromycin, and azithromycin.
You’ve probably taken at least one of these before. These medications are processed through your liver using the same pathways as cannabis. This creates potential competition.
When I take a macrolide antibiotic, my liver works harder to break down both substances. This can lead to stronger or longer-lasting effects from cannabis. It might also increase side effects from the antibiotic itself.
Some people experience unpredictable reactions they weren’t expecting. But wait, there’s good news too. Doxycycline shows minimal interference with cannabis.
Research suggests this antibiotic doesn’t compete for the same liver enzymes. That sounds reassuring, right? Still, “minimal” doesn’t mean zero risk. Every person’s body processes medications differently.
Your safest bet? Talk to your pharmacist about your specific antibiotic before making any decisions. They know the exact medication you’re taking.
Why Smoking Is Particularly Risky During Illness

Here’s where things get more serious. Smoking while you’re already sick creates extra problems. If you have a respiratory infection, smoking makes everything worse. Your lungs are already fighting bacteria or inflammation.
Adding smoke is like throwing gasoline on a fire. Think about what happens when you smoke. Hot smoke irritates your throat and lung tissue. This irritation slows down your body’s natural healing process.
I’ve seen patients turn simple bronchitis into pneumonia because they kept smoking during treatment. Your immune system works overtime when you’re sick. Smoking forces it to handle additional toxins instead of focusing on getting you better.
Recovery time doubles or triples in many cases. Consider Sarah, a 28-year-old with strep throat. She continued smoking throughout her antibiotic course. What should have been a five-day recovery stretched to two weeks of persistent symptoms.
How Cannabis Affects Antibiotic Metabolism
Cannabis may influence how your body processes antibiotics by affecting liver enzymes, possibly altering drug absorption, potency, or side effects.
Liver Enzyme Interactions
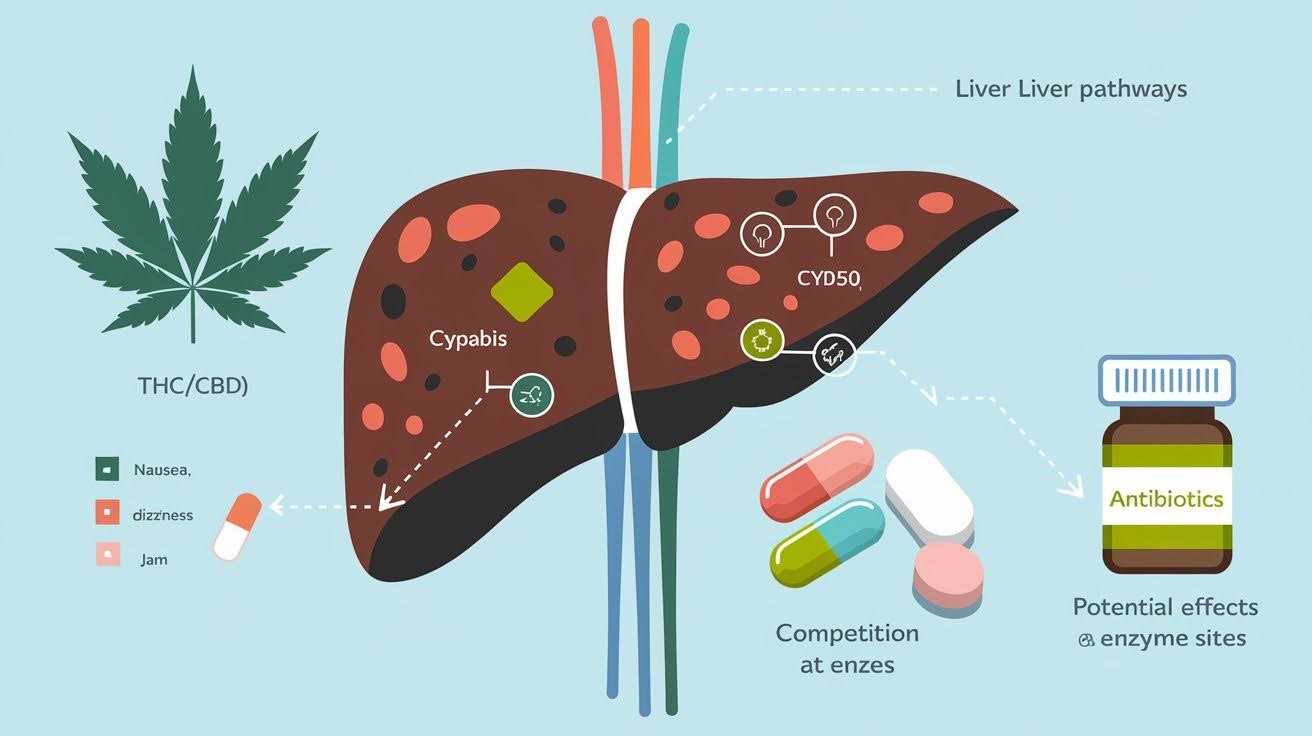
Your liver acts like a processing plant for everything you put in your body. It breaks down medications using special enzymes. These enzymes work like tiny machines. They take complex substances and turn them into simpler forms your body can handle or remove.
When I consume cannabis, both THC and CBD compete for the same enzymes that process many antibiotics. This creates a traffic jam in your liver. Think of it this way. You have one checkout lane at the grocery store, but two customers are trying to pay at once.
The result? Your antibiotic might stay in your bloodstream longer than expected. Higher levels can mean stronger side effects. Some people experience nausea or dizziness that they wouldn’t normally get. Others find their medication works differently than usual.
The effects can last several hours longer than your doctor planned. Your body simply can’t keep up with processing both substances efficiently.
Documented Side Effects of Combining Cannabis and Antibiotics
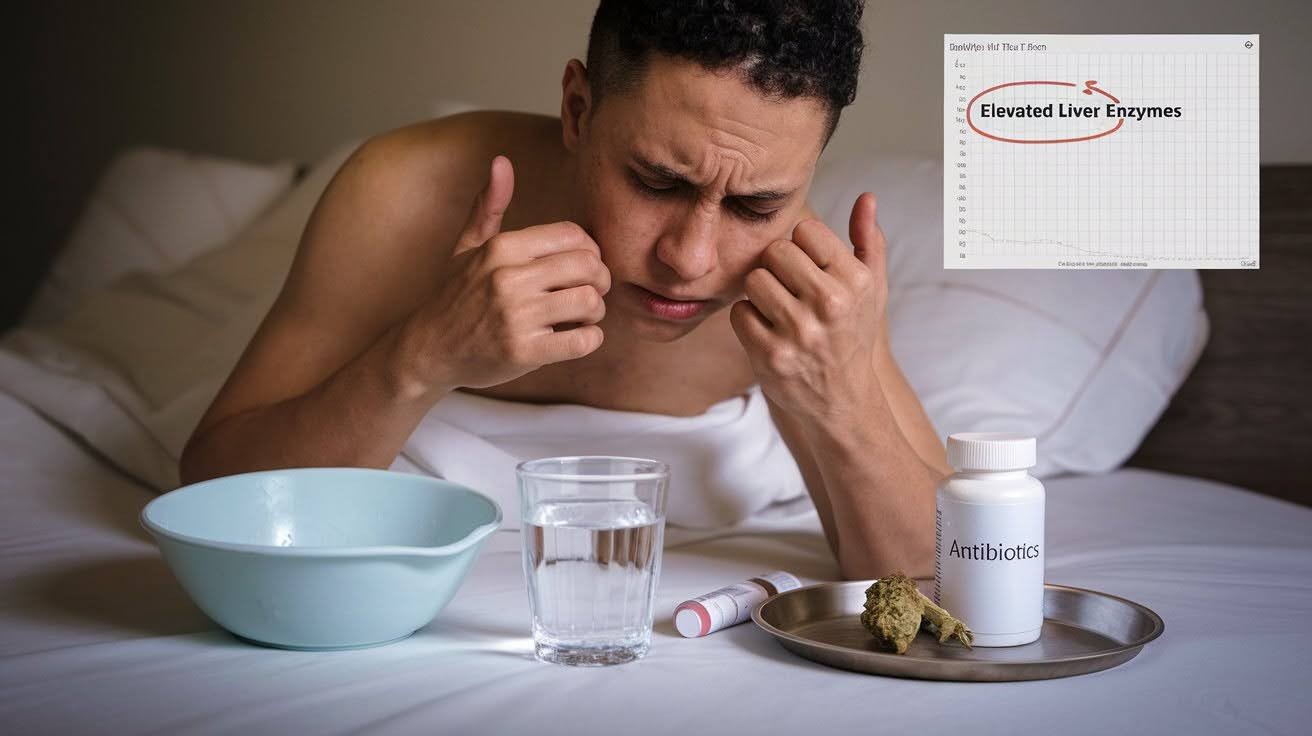
The combination can amplify problems you might already face with antibiotics alone. Nausea becomes much worse when both substances hit your system together. I’ve heard from patients who couldn’t keep food down for days. What started as a mild stomach upset turned into serious vomiting episodes.
Diarrhea also increases significantly. Your digestive system struggles to handle the double impact. This can lead to dangerous dehydration.
Your liver bears the biggest burden. Processing both cannabis and antibiotics simultaneously puts extra stress on this vital organ. Some people develop elevated liver enzymes, which show up in blood tests.
Mood changes catch people off guard, too. Anxiety spikes unexpectedly. Some feel paranoid or confused in ways they’ve never experienced before.
Seek medical help immediately if you experience severe vomiting, can’t keep fluids down, develop yellowing skin or eyes, or feel extremely confused. These signs indicate serious complications.
Safer Alternatives to Smoking During Antibiotic Treatment
Consider safer alternatives like edibles, tinctures, or topicals during antibiotic treatment. These methods avoid lung irritation and reduce interaction risks.
Non-Smoking Cannabis Options

If you need cannabis while taking antibiotics, smoking isn’t your only choice. Sublingual tinctures offer a gentler approach. You place drops under your tongue and hold them there for 30 seconds. Cannabis absorbs directly into your bloodstream without passing through your lungs or liver first.
This method bypasses much of the interaction risk. Topical creams and balms work well for localized pain or inflammation. They affect only the area where you apply them. Your bloodstream barely absorbs these products.
But here’s something important about edibles. I don’t recommend them during antibiotic treatment. Edible cannabis goes straight to your liver for processing. Remember that traffic jam we talked about earlier?
Edibles make it much worse. Your liver already works overtime processing antibiotics. Adding edible cannabis creates the exact problem we’re trying to avoid. Stick with tinctures or topicals if you must use cannabis.
CBD vs. THC Considerations

CBD offers a safer path than THC when you’re taking antibiotics. It doesn’t get you high, which removes one layer of unpredictability from the equation. CBD can help manage pain, reduce inflammation, and calm anxiety without the psychoactive effects. Your body processes it differently than THC, too.
But here’s the catch. Even CBD interacts with liver enzymes, just less aggressively than THC. Lab-tested products become crucial during this time. You need to know exactly what you’re putting in your body.
Street products or untested items contain unknown chemicals that could create dangerous interactions. Stick with certified, third-party tested CBD if you choose this route.
Dosage and Safety Guidelines

Start smaller than you normally would. Your body handles substances differently when fighting infection. I recommend cutting your usual dose in half initially. See how you feel before taking more.
Avoid trying new cannabis products while on antibiotics. This isn’t the time for experimentation. Stick with brands and types you’ve used successfully before. Monitor yourself closely for any unusual symptoms. Keep a simple log of how you feel each day.
Watch for increased nausea, unexpected dizziness, or unusual fatigue. These signs suggest the combination isn’t working well for your body. If something feels off, stop using cannabis immediately and contact your healthcare provider.
When to Consult Healthcare Providers
Consult healthcare providers if you experience side effects, delayed recovery, or plan to use cannabis alongside antibiotics for safe guidance.
Essential Medical Consultations

Your prescribing doctor needs to know about your cannabis use. I know this conversation feels awkward, but it’s essential for your safety. Most physicians won’t judge you. They need complete information to make the best treatment decisions for your specific situation.
Your pharmacist is another valuable resource. They understand drug interactions better than almost anyone. Many pharmacists have specialized training in cannabis interactions, too. Don’t feel embarrassed about asking questions. Pharmacists deal with these concerns daily.
If you have a medical marijuana doctor, contact them as well. They understand both sides of the equation and can provide specific guidance for your condition and medication combination.
Warning Signs Requiring Immediate Attention

Some symptoms demand immediate medical care. Don’t wait or hope they’ll improve on their own. Severe stomach pain, persistent vomiting, or blood in your stool signal serious digestive problems. Your body might be rejecting the combination.
Unusual anxiety attacks or mood swings that feel different from normal cannabis effects need attention. This suggests your brain chemistry is being affected unexpectedly. Yellowing skin or eyes, dark urine, or extreme fatigue point to liver problems. These symptoms can become life-threatening quickly.
Difficulty breathing, chest tightness, or facial swelling indicate allergic reactions. Call emergency services immediately if you experience these symptoms. Trust your instincts. If something feels seriously wrong, seek help right away.
Conclusion
The question “Can you smoke while on antibiotics?” doesn’t have a simple yes or no answer. Your safety depends on multiple factors: the type of antibiotic you’re taking, your current health status, and what kind of infection you’re treating.
Smoking anything while sick puts extra stress on your body when it needs to focus on healing. The smart choice is waiting until you finish your antibiotic course. If you need cannabis for medical reasons, safer alternatives like tinctures or topicals can reduce your risk significantly.
You now have the facts to make an informed decision that puts your health first. Remember, your doctor and pharmacist are always your best resources for personalized advice. Have questions about your specific situation? Drop a comment below, we’re here to help you stay safe while getting better.
Frequently Asked Questions
Can you smoke while on antibiotics?
It’s generally not recommended. Smoking can interfere with your body’s healing process and may interact with certain antibiotics, particularly macrolides like azithromycin and erythromycin.
What happens if I smoke cannabis while taking antibiotics?
Cannabis and antibiotics both pass through your liver, potentially causing increased side effects like nausea, dizziness, or prolonged medication effects in your bloodstream.
Are some antibiotics safer to smoke with than others?
Doxycycline shows minimal cannabis interactions, while macrolide antibiotics (erythromycin, clarithromycin, azithromycin) carry higher risks due to competing liver pathways.
How long should I wait to smoke after finishing antibiotics?
Wait at least 24-48 hours after your final antibiotic dose to ensure the medication has cleared your system and won’t interact with cannabis.
What’s the safest way to use cannabis while on antibiotics?
If necessary, choose CBD tinctures or topical products over smoking. Avoid edibles and always consult your doctor or pharmacist first for personalized advice.